The risks of developing Alzheimer’s and Parkinson’s diseases, as well as other neurodegenerative disorders, are influenced by a combination of genetic susceptibility and environmental factors. Although certain genetic mutations increase the risks of developing these conditions, not everyone who carries such mutations will develop them.
We have discovered four common pathogenic mechanisms by which bacteriophages are implicated in different neurodegenerative disorders. These latest discoveries from HMI will allow us to rethink how we treat and prevent neurodegenerative diseases and to find new approaches to improve their therapy to a new level of efficacy.
HMI is working on breakthrough therapies by focusing on the use of bacteriophages as previously overlooked therapeutic targets.
Implication of phages in neurodegeneration:
Propagation of Protein Misfolding
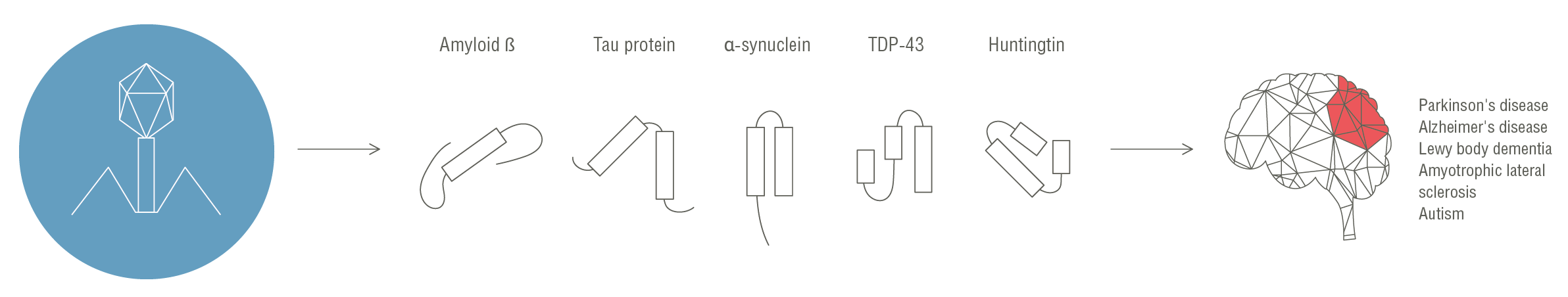
Protein misfolding and the formation of prions has become the leading theoretical mechanism for the development of multifaceted autoimmune and neurodegenerative disorders such as Parkinson’s and Alzheimer’s diseases, amyotrophic lateral sclerosis, type 1 diabetes, etc. HMI’s world-class team has for the first time identified various prion-like domains that have a strong capability to become prions in multiple bacteriophages, including those associated with the human microbiota. The involvement of these bacteriophage prion domains in cross-kingdom interactions with eukaryotic protein misfolding is currently being investigated by HMI.
Phage-Induced Alterations in the Abundances of Certain Bacteria Might Trigger Human Diseases
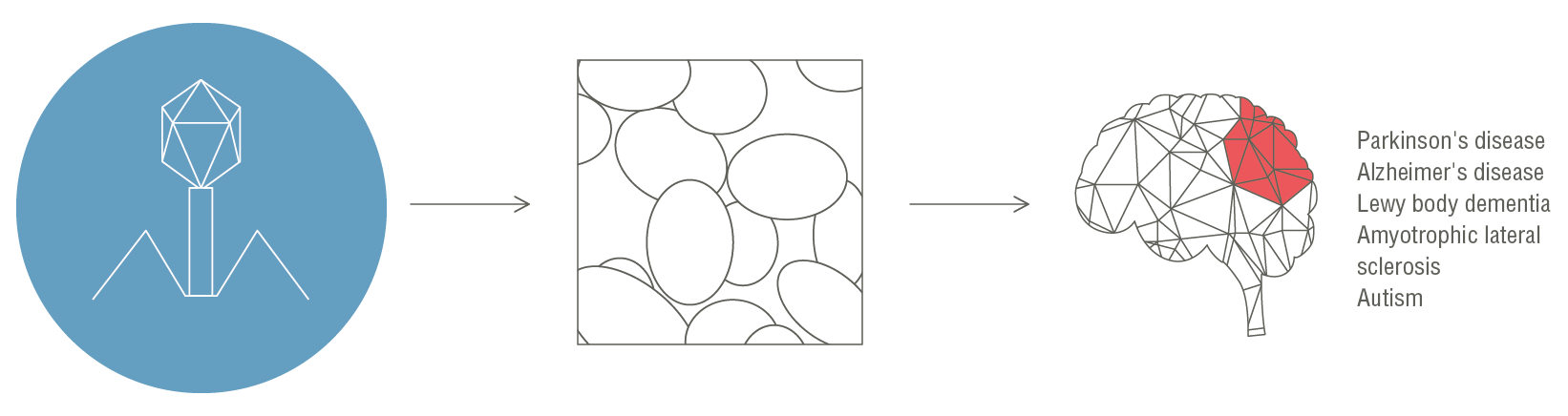
Bacteriophages can interact with bacteria through lytic and lysogenic infection modalities, both of which can lead to the lysis of bacterial host cells, significantly altering the abundances of certain bacteria and thereby indirectly contributing to the shift from health to disease in mammals.
In patients with Parkinson’s disease, HMI recently discovered elevated levels of lytic bacteriophages, contributing to a significant functional alteration of the microbiome that is most likely to be associated with the onset of pathology. We believe that the same alterations may also be associated with other neurodegenerative diseases.
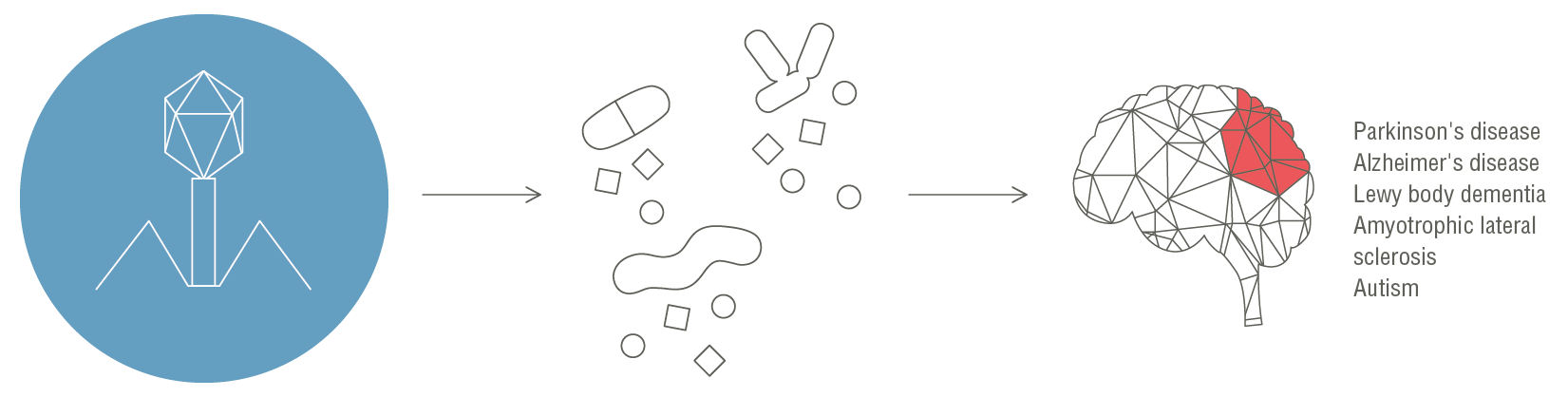
Bacteriophages Induce Elevated Levels of Pathogen-Associated Molecular Patterns (PAMPs)
In our work, we showed that bacteriophages induce increased levels of plasma cell-free bacterial DNA and other PAMPs such as lipopolysaccharides, peptidoglycan, and bacterial amyloid, which can enter the blood circulation, particularly in subjects with a substantially increased intestinal permeability. Given that an increased gut permeability facilitates the translocation of PAMPs into the circulation, under certain conditions particular bacteriophages might simultaneously induce gut leakiness and cause bacterial lysis, leading to elevated serum PAMP levels.
The phage-induced increase in intestinal permeability
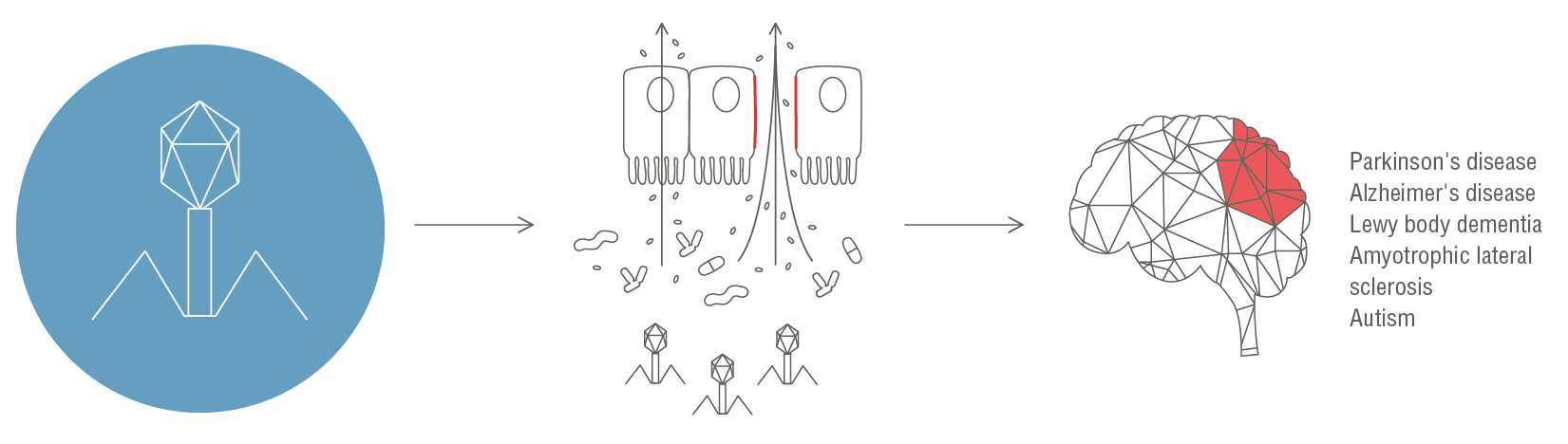
We discovered that certain bacteriophages increase intestinal permeability, leading to the translocation of gut bacteria and facilitating chronic inflammation and an altered immune response, thus triggering various neurodegenerative and autoimmune diseases.